What are the Surgical and Non-Surgical Modalities Utilized in the Management of Various Stages of Decubitus Ulcers?
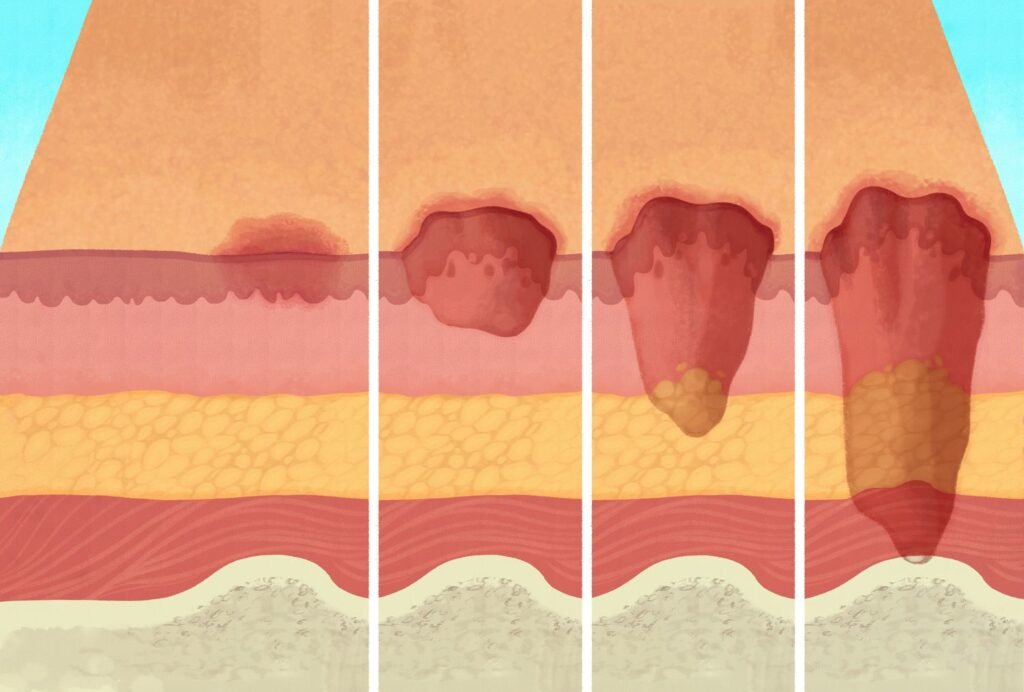
Daniel Davidson, MD, MBA, DBA, PHD Introduction: Decubitus ulcers—also referred to as bedsores or pressure ulcers—pose a serious risk to patient safety and quality of life, making them a major healthcare concern. Decubitus ulcer treatment necessitates a multimodal strategy, with potential surgical and non-surgical interventions based on the ulcer’s particular stage. This article examines the range of surgical and non-surgical procedures used to treat decubitus ulcers at different phases of the condition. Stage-Based Management: The method of treating decubitus ulcers according to the degree of the wound—which is divided into stages that range from Stage I to Stage IV—is known as “stage-based management.” To encourage healing and stop more issues, each stage denotes a distinct degree of tissue involvement and calls for particular therapies. Stage I: Stage I ulcers are superficial sores that impact the skin’s outermost layer. The skin doesn’t break even if it looks red.Management and oversight: Put prevention first: By using pressure-relieving surfaces and relocating the damaged area, you can stop more harm from occurring.Preserve the integrity of your skin: Prevent the skin from going to deeper stages by keeping it hydrated, free of friction, and clean. Stage II: Stage II ulcers are characterized by a partial thickness loss of epidermal integrity that penetrates into the dermis. The injury could manifest as a shallow crater, blister, or abrasion.Supervisory: Wound care: To keep the wound moist and encourage healing, use the proper dressings. In addition to absorbing extra fluid, dressings should shield the wound from additional harm.Offload pressure: To stop additional tissue injury and promote recovery, keep up the pressure relief measures. Stage III: Stage III ulcers are characterized by a complete loss of epidermal integrity that extends into the subcutaneous region. The incision might resemble a large crater with visible fat.Supervisory: Debridement of the wound: In order to encourage healing and guard against infection, remove any necrotic or non-viable tissue from the ulcer site.Control of infections: Keep an eye out for symptoms, and if necessary, start the right antibiotic treatment.Offload pressure: To reduce pressure at the ulcer site, keep applying pressure relief techniques and make use of specific support surfaces. Stage IV: The most severe type of ulcers, known as stage IVs, entail full-thickness tissue loss that spreads into the muscle, bone, or supporting structures. A deep crater with exposed muscle, bone, or tendon may be the appearance of the wound.Surgical intervention: To encourage wound closure and tissue regeneration, take into account surgical methods such flap reconstruction, skin grafting, or tissue transfer operations.Wound vacuum therapy: By eliminating extra fluid and encouraging the growth of granulation tissue, negative pressure wound therapy (NPWT) helps to accelerate wound healing.Intensive wound care: To avoid problems and encourage healing, give careful wound care and infection control measures. Surgical Modalities: Surgical techniques are essential interventions in the management of decubitus ulcers, especially when the ulcers are progressed and non-surgical treatments may not be adequate. The goals of these surgical methods are to stop additional problems, seal the ulcer site, and encourage wound healing. Now let’s examine the many surgical techniques frequently applied to the treatment of decubitus ulcers: Rebuilding the Flaps:During a surgical process called flap reconstruction, healthy tissue from nearby parts of the body, such as skin, subcutaneous fat, and occasionally muscle, is transferred to cover the ulcer site. This procedure is especially helpful for large, complicated, or deep ulcers where conventional wound closure techniques might not be sufficient. Benefits:Gives the ulcer location a strong, well-vascularized tissue covering.Contributes to the healing of wounds by supplying healthy tissue with an unbroken blood flow.Lowers the chance of a wound healing poorly and returning. Flap Types: Rotational Flaps: To cover the ulcer location, tissue is rotated in from surrounding areas. Because of their versatility, rotational flaps can be made to fit the exact size and form of the wound.Advancement Flaps: To cover the ulcer, tissue is moved forward from nearby regions. To achieve tension-free closure and close larger faults, advancement flaps can be helpful. Skin Grafting:The goal of skin grafting is to encourage tissue regeneration and wound closure by transplanting healthy skin from a donor site to the ulcer site. Depending on how deeply tissue is taken, skin grafts can be divided into full-thickness or split-thickness categories. Benefits:Offers a comparatively easy and efficient way to seal wounds.Can be taken from a variety of donor locations, including as the patient’s own body (autograft), cadaveric sources (allograft), or artificial materials (xenograft).Encourages the healing of wounds and re-epithelialization. Skin Graft Types: Split-Thickness Skin Grafts: These skin grafts are made up of some dermis and some epidermis. When there is a enough supply of donor skin, they are frequently used for bigger wounds.Full-Thickness Skin Grafts: The complete dermis and epidermis are grafted in these cases. They work well for smaller, shallower wounds and yield superior esthetic results. Procedures for Tissue Transfer: In order to encourage wound healing and tissue regeneration, vascularized tissue, such as muscle or fasciocutaneous flaps, is transplanted to the ulcer site during tissue transfer procedures. When there is underlying tissue loss in deep or widespread ulcers, these methods are especially helpful. Benefits:Gives densely vascularized tissue a steady blood supply, which encourages quick healing and lowers the chance of graft failure.Able to treat intricate wound flaws that expose bone or muscle.Lowers the chance of recurrence and provides long-lasting coverage. Non-Surgical Modalities: When it comes to the treatment of decubitus ulcers, non-surgical techniques are quite important, especially in the initial phases of wound development. Without requiring intrusive procedures, these therapies aim to stop more tissue damage, encourage wound healing, and lower the risk of complications. Pressure release: Pressure release is essential for stopping decubitus ulcers from getting worse. Blood flow to the injured tissues is enhanced by lessening pressure on sensitive parts of the body, such as bony prominences, which promotes healing and stops additional harm. Repositioning the patient on a regular basis, using cushions or mattresses that relieve pressure points, and maximizing patient mobility are all strategies for pressure reduction.Skin Maintenance: Maintaining skin integrity and halting